Hypertensive retinopathy (HR) refers to changes in the retinal microvasculature that occur due to elevated blood pressure. It is a significant complication of uncontrolled hypertension and serves as a visible manifestation of systemic vascular damage, indicating pathology that affects the entire body.
Indications (Clinical Signs)
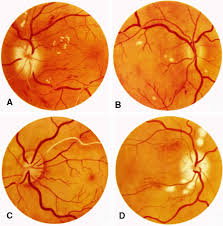
HR progresses through various stages, with observable changes in the fundus (the back of the eye). These signs can be graded, for example, using the Keith-Wagener-Barker classification:
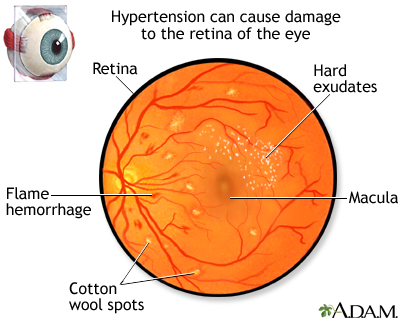
- Arteriolar Narrowing: This is often the earliest sign, with a mild generalized arterial attenuation in Grade 1. More marked generalized and focal narrowing, along with arterio-venous nicking (AVN) (where arterioles compress venules at crossing points), appear in Grade 2.
- Vessel Wall Changes: In more advanced stages (Grade 3), “copper-wiring” of arterioles and changes like Bonnet and Gunn signs are observed. “Silver wiring” of arterioles is characteristic of Grade 4.
- Hemorrhages: Blot and flame-shaped hemorrhages can be present, typically in Grade 3 and higher.
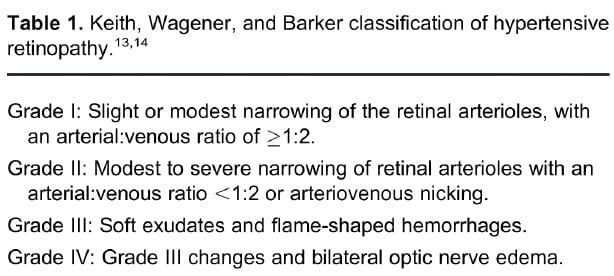
- Exudates: Hard exudates (lipid residues) and cotton wool spots (fluffy white patches from nerve fiber damage due to ischemia) are significant findings in moderate to severe HR (Grade 3 and 4).
- Optic Disc Edema (Papilledema): Swelling of the optic disc, indicating severe or malignant HR (Grade 4 or malignant stage), is a critical sign.
- Vascular Tortuosity: A twisting and curving of retinal blood vessels may also be noted.
- Other Findings via OCT: Spectral-domain optical coherence tomography (SD OCT) can reveal hyperreflective dots, subretinal fluid (SRF), and intraretinal fluid (IRF), as well as thickening or wrinkling of the nerve fiber layer, and disruption of the photoreceptor layer.
Symptoms
Patients with HR may experience various ocular and systemic symptoms:
- Blurred Vision/Reduced Vision: This is a common complaint, potentially bilateral. Vision loss can be gradual and painless.
- Headache: An unusual headache may be reported.
- Other Ocular Morbidities: HR can be associated with complications such as sub-conjunctival hemorrhage, retinal vein or artery occlusion, ischemic optic neuropathy, and cranial nerve palsy.
- Mental and Psychological Disorders: Long-term visual impairment in HR patients can lead to anxiety and depression, with altered spontaneous brain activity patterns observed in specific brain regions.
Management
The management of HR primarily focuses on controlling the underlying high blood pressure to prevent further ocular and systemic damage:
- Immediate Blood Pressure Control: For hypertensive emergencies (systolic BP ≥ 180 mmHg or diastolic BP ≥ 120 mmHg with target organ damage), immediate emergency department admission and antihypertensive treatment are critical.
- Medication Adherence: Poor adherence to prescribed hypertensive medications is associated with a higher likelihood of HR.
- Routine Eye Examinations: Regular eye check-ups are essential for patients with high blood pressure to detect and manage retinal damage early. The eye can serve as an “observation window” for potentially fatal end-organ damage.
- Lifestyle Modifications: A balanced diet and regular exercise are important for effective blood pressure management.
- Multidisciplinary Approach: Hypertensive patients should ideally be managed holistically by both a medical doctor and an ophthalmologist to prevent visual impairment.
- Monitoring and Follow-up: With effective blood pressure control, retinal and choroidal changes often show significant improvement. However, subtle changes may remain detectable even after a year. Long-term follow-up is important to monitor residual changes and visual outcomes.
- Emerging Therapies: Research explores new approaches, such as the use of Fucoidan (FO), a fucose-enriched sulfated polysaccharide, which has shown potential to mitigate retinopathy by modulating the SIRT1/NLRP3 pathway, influencing inflammation and oxidative stress.
Outcomes of Medical Treatment
- Resolution of Ocular Signs:
Macular edema with subretinal fluid (SRF) is a primary cause of mild-to-moderate vision reduction upon presentation, and these signs typically resolve with antihypertensive medications. Retinal hemorrhages and cotton wool spots can show near-complete resolution. Subretinal fluid and intraretinal fluid often resolve entirely within three months of initiating antihypertensive therapy, although hyperreflective dots may persist for a longer duration. Some degree of vessel tortuosity might remain observable even after treatment.
- Visual Improvement:
The improvement in mean BCVA at three months was statistically significant2…. Changes in SBP, DBP, mean arterial pressure (MAP), and subfoveal choroidal thickness (SCT) correlated significantly with visual outcomes.
- Incomplete Visual Recovery:
While significant improvement is common, complete visual recovery can be incomplete due to factors such as macular ischemia, exudative retinal detachment (RD), optic neuropathy, loss of photoreceptor layer integrity, residual hard exudates, and macular thinning. Photoreceptor layer integrity is considered an independent prognostic factor.
- Systemic Indicators:
HR is positively correlated with albuminuria (a biomarker for early kidney injury), indicating that HR can be used as an indicator of early renal injury. With the aggravation of HR, albuminuria becomes more obvious, and renal damage more serious.
- Psychological Impact:
Long-term visual impairment in HR patients can lead to mental and psychological disorders, such as anxiety and depression, which have been correlated with altered spontaneous brain activity patterns in specific brain regions.
.
References
- Eppenberger LS, Schmid MK, Clerici M. Acute Ocular Complications af. Klin Monatsbl Augenheilkd. 2023;240:505–508.
- Fieß A, Gißler S, Wild PS, Lackner KJ, Münzel T, Michal M, et al. Hypertensive Retinopathy is Not Associated with Low or High Birth Weight – Results from the Population-Based German Gutenberg Health Study. Clin Ophthalmol. 2024;18:1797–1800.
- Gudayneh YA, Seid A, Gebeyehu A, Negash A, Yeshambel B, Gobena A, et al. Prevalence of hypertensive retinopathy and associated factors in adult hypertensive patients attending at Comprehensive Specialized Hospitals in Northwest Ethiopia in 2024. Int J Retina Vitreous. 2025;11:17.
- Kankrale R, Kokare M. Artificial intelligence in retinal image analysis for hypertensive retinopathy diagnosis: a comprehensive review. Visual Computing for Industry, Biomedicine, and Art. 2025;8:11.
- Khoshtinat et al. Association of hypertensive disorders of pregnancy and gestational diabetes mellitus with retinopathy of prematurity: a comparative analysis. Int J Retina Vitreous. 2025;11:52.
- Li J, Zhang W, Zhao L, Zhang J, She H, Meng Y, et al. Positive correlation between hypertensive retinopathy and albuminuria in hypertensive adults. BMC Ophthalmol. 2023;23:66.
- Li J, Wang X, Bai J, Wei H, Wang W, Wang S. Fucoidan modulates SIRT1 and NLRP3 to alleviate hypertensive retinopathy: in vivo and in vitro insights. J Transl Med. 2024;22:155.
- Mishra P, Kanaujia V, Kesarwani D, Sharma K, Nanda J, Mishra P. Visual Outcomes in Malignant Hypertensive Retinopathy Cases: A Clinical and Spectral Domain Optical Coherence Tomography Study. Cureus. 2024;16(6):e62945.
- Nam KY, Lee MW, Jun JH, Sung JY, Kim JY. Different characteristics of retinal damage between chronic hypertension and hypertensive retinopathy. Sci Rep. 2022.
- Wang XL, Zheng XJ, Zhang LJ, Hu JY, Wei H, Ling Q, et al. Altered spontaneous brain activity patterns in hypertensive retinopathy using fractional amplitude of low-frequency fluctuations: a functional magnetic resonance imaging study. Int J Ophthalmol. 2024;17(9):1665–1674.
- Wang XL, Chen Y, Hu JY, Wei H, Ling Q, He LQ, et al. Alterations of interhemispheric functional connectivity in patients with hypertensive retinopathy using voxel-mirrored homotopic connectivity: a resting state fMRI study. Int J Ophthalmol. 2025;18(2):297–307.
- Zamaladi I, Ruvuma S, Mceniery CM, Kwaga T, Wilkinson IB, Atwine D, et al. Retinopathy among women with hypertensive disorders of pregnancy attending hospitals in Mbarara city, south-western Uganda: a cross-sectional study. BMJ Open. 2023;13:e076365.
Keywords
Hypertension (HTN), Elevated Blood Pressure, Ocular Impact, Optic Disc Edema / Papilledema, Cotton Wool Spots, Retinal Hemorrhages, Hard Exudates, Splinter Bleeding, Cystoid Macular Edema (CME), Subretinal Fluid (SRF), Intraretinal Fluid (IRF), Arteriovenous Nicking (AVN), Vascular Tortuosity, Elschnig Spots, Exudative Retinal Detachment (RD)