Visual field defects classification
Classification by Pattern and Location of Damage: The pattern of visual field loss often correlates with the location of the damage in the visual pathway, which extends from the eye to the brain.
- Homonymous Visual Field Defects (HVFDs): These involve vision loss in the same half (left or right) of the visual field in both eyes. They are typically caused by lesions after the optic chiasm, such as stroke, brain tumors, or traumatic brain injuries.
- Hemianopia (or Hemianopsia): Loss of vision in half of the visual field. This can be left or right-sided.
- Quadrantanopia: Loss of vision in a quarter of the visual field (e.g., upper or lower quadrant)1…. The sources mention a case of monocular right lower quadrantanopia.
- Paracentral Scotoma: Loss of vision in the paracentral visual fields of both eyes, appearing as dark spots near the center.
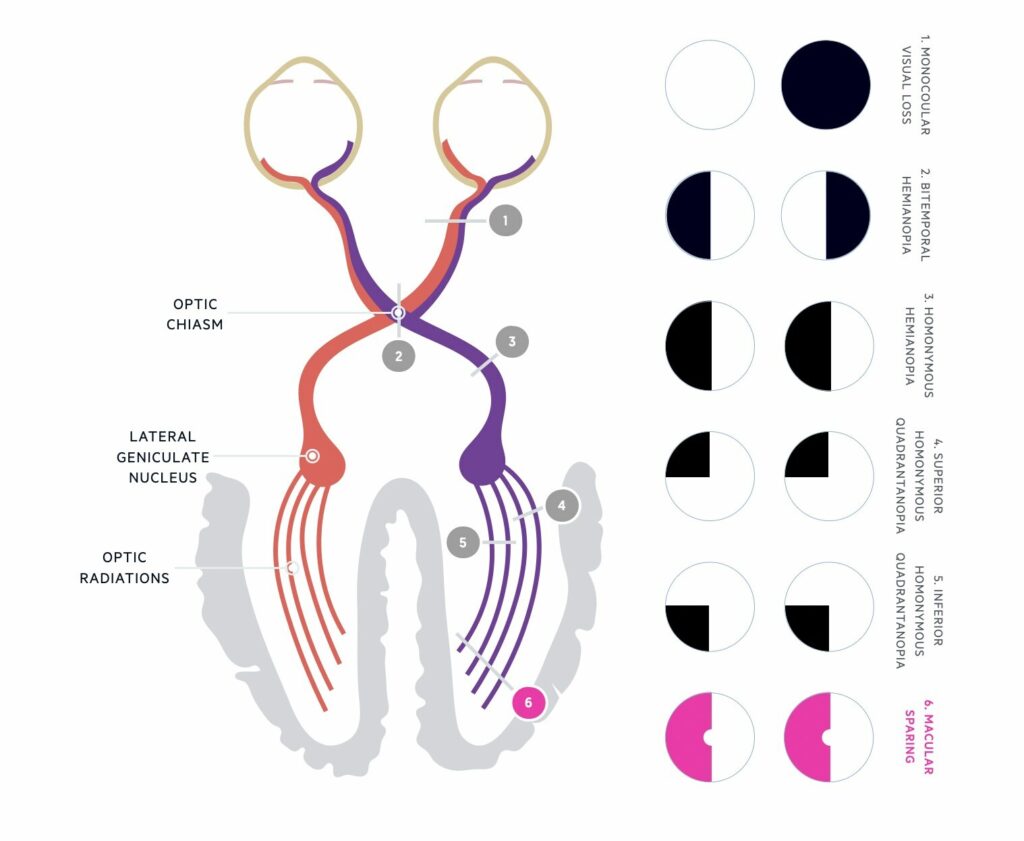
- Bitemporal Hemianopsia: Loss of vision in the outer halves of both visual fields, characteristic of damage to the optic chiasm.
- Defects related to Optic Tract, Optic Radiation, and Visual Cortex injury: These typically manifest as homonymous hemianopsia.
- Defects related to the Optic Nerve: Primary open-angle glaucoma (POAG) causes progressive loss of retinal ganglion cells and axons, leading to characteristic optic nerve head changes and corresponding visual field defects. Optic Nerve Head Drusen (ONHD) are also strongly related to visual field defects.
Classification by Specific Shapes/Patterns in Glaucoma and Other Conditions:
- Arcuate Scotoma: An arc-shaped area of vision loss. Sources mention superior arcuate scotoma, inferior arcuate scotoma, and double arcuate scotoma in POAG and it is also seen with ONHD.
- Nasal Step: A step-like defect on the nasal side of the visual field.
- Tubular Vision: Severe constriction of the visual field, leaving only central vision.
- Concentric VF Constriction: A general shrinking of the outer boundaries of the visual field.
- Enlarged Blind Spot: The naturally occurring blind spot becomes larger.
- Generalized Visual Field Defect: A general reduction in sensitivity across the visual field.
- Localized Visual Field Defect: Vision loss confined to a specific area.
- Unspecific Visual Field Defects: Defects that don’t fit into typical patterns.
- Abnormal Clusters: Specific groupings of points with reduced sensitivity, used in criteria for diagnosing glaucomatous visual field abnormalities.
Classification by Severity:
In glaucoma, severity is commonly graded based on the Mean Deviation (MD) index from visual field tests and the pattern of loss. Severity grades mentioned include:
- Mild Glaucoma: Often characterized by a nasal step or paracentral scotoma with MD less than -6 dB20.
- Moderate Glaucoma: Characterized by an arcuate scotoma with MD between -6 dB and -12 dB20.
- Severe Glaucoma: Involves extensive field loss, including defects within the central 10 degrees, with MD greater than -12 dB20.
- End-stage Glaucoma: Cases where visual field testing is difficult or impossible due to a central scotoma.
Hodapp-Parrish-Anderson (HPA) criteria:
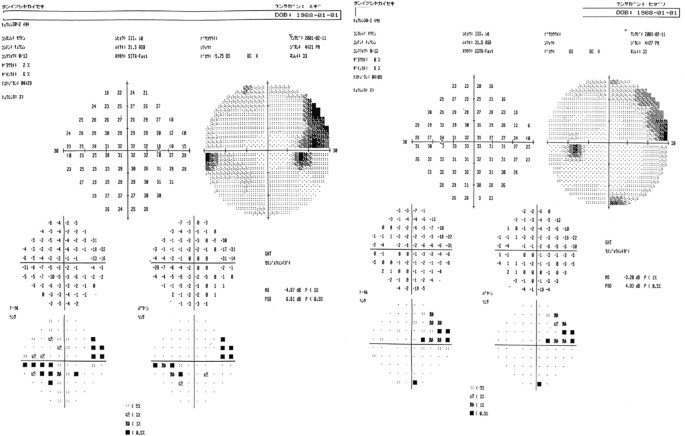
The Hodapp-Parrish-Anderson (HPA) criteria provide standardized rules for classifying glaucomatous visual field defects as ‘early’, ‘moderate’, and ‘severe’ based on Mean Deviation, the global plot, and the pattern deviation on Humphrey visual field test printouts.
Early detection and precise measurements
VFDs are crucial for the diagnosis and management of both ophthalmological (like glaucoma) and neurological diseases.
- Different techniques are used to assess visual fields, including Standard Automated Perimetry (SAP) using machines like the Humphrey Field Analyzer (HFA) or Octopus, microperimetry (e.g., MAIA) which combines fundus imaging with gaze-contingent stimulus presentation for more precise assessment, confrontation visual field testing, and objective methods based on electrophysiology like Visual Evoked Potentials (VEP) or multifocal VEP (mfVEP) and pupillometry. Newer, low-cost grid tests like the TsiogkaSpaeth (TS) grid are also being explored for screening and detecting neurological VFDs.
- In glaucoma, interpretation of visual fields is essential for diagnosis, severity grading, and prognostication. Staging glaucomatous field defects is also an important component of risk stratification. The GFDC application, as discussed, automates the Hodapp-Parrish-Anderson (HPA) criteria for this purpose, aiming to improve the accuracy, reliability, and fairness of visual field assessment by standardizing the process and overcoming subjectivity.
- Regular follow-up with automated perimetry evaluation (often every 6 months until stabilization, then annually) is part of patient management, for instance, in cases of optic nerve head drusen (ONHD). The TS grid test is also suggested as potentially useful for monitoring visual field defects of neurologic origin.
- Patient Education and Support: Making patients aware of their visual field abnormalities can be important. It may motivate them to seek medical care for early diagnosis, help them understand their condition, improve adherence to topical therapy, and facilitate informed consent for surgery.
In summary, managing visual field defects involves comprehensive assessment and monitoring using various perimetric techniques, careful differential diagnosis, standardized severity grading (especially in glaucoma), and targeted rehabilitation or therapeutic interventions, particularly for acquired defects like HVFDs, alongside patient education. Tools that improve the objectivity and accessibility of visual field assessment, such as automated HPA classification or portable screening tests, are seen as valuable contributions to patient management.
References
- Bolognini N, Casati C, Falsini S, Trimboli F, Stampatori C, Dacquino L, et al. Telerehabilitation for visual f[ield defects] 2025.
- Cai Y, Strauch C, van der Stigchel S, Ten Brink AF, Cornelissen FW, Naber M. Mapping simulated visual field defects 2025.
- Ganguli MP, Robinson E, Kile MR, Kapp D. Bilateral Optic Disk Swelling and Peripheral Visual Field Defects as a Rare Initial Presentation of Primary Chiari I Malformation 2023 Jun 19.
- Hanai Y, Morita N, Nishida M, Nakayama N, Miyake S, Tsumura A, et al. Tuberculum meningioma with recovery. BMC Ophthalmol. 2024;24:68.
- Inoue A, Matsumoto C, Koike E, Maeda N. Subjective perception of visual fie[ld defects] 2024.
- Maeyama T, Okada H, Sakai S. The effects of rehabilitative interventions on reading disorders caused by homonymous visual field defects : a meta-analysis focusing on improvement in reading speed. Acta Neurol Belg. 2023;124:123-140. doi:10.1007/s13760-023-02327-6.
- Mudhol RR, Ray A, et al. Exploring the Relation Between Peripheral retinal vasculature and visual field defects 2024.
- Redmond BV, Fahrenthold BK, Yang J, Saionz EL, Cavanaugh MR, Huxlin KR. MAIA and Humphrey Perimetry Differ in their Estimation of Homonymous Visual Field Defects. Transl Vis Sci Technol. 2024;13(11):15. doi:10.1167/tvst.13.11.15.
- Tol SV, et al. Reading Difficulties in Individuals w[ith homonymous visual field defects] 2024.
- Tsiogka A, Moster ML, Chatzistefanou KI, Karmiris E, Samoli E, Giachos I, et al. The TsiogkaSpaeth grid for detection of neurological visual field defects: a validation study. Neurol Sci. 2024;45:2869–2875. doi:10.1007/s10072-024-07305-1.
- Tsiogka A, Moster ML, Chatzistefanou KI, Karmiris E, Samoli E, Giachos I, et al. Diagnostic accuracy of the TsiogkaSpaeth grid for visual field defects in glaucoma patients: a validation study. BMJ Open Ophthalmol. 2025.
- Yamaguchi C, Kiyota N, Takahashi N, Takeda Y, Omodaka K, Tsuda S, et al. Factors associated with intrach[oroidal cavitation] 2024.